The Saga of PI3K Inhibitors: Part 2 – The shifting role of overall survival
In Part 1 of our blog series on the saga of PI3K inhibitors, we reviewed the FDA’s recent Oncologic Drugs Advisory Committee (ODAC) meeting on April 21, 2022, to discuss the agency’s concerns about PI3K inhibitors (PI3Kis). The panel voted resoundingly (16 yes votes; 1 abstention) that future approvals of PI3Kis should be supported by randomized data that would allow an assessment of overall survival (OS)—an action that makes accelerated approvals less likely and more difficult to obtain in slow-growing cancers with a long median survival.
At the heart of the FDA’s concerns with the PI3Ki class is an apparent excess of deaths in clinical trials of PI3Kis, indicating a potential detriment to long-term survival in patients who were treated with PI3Kis. However, assessing OS in patients with indolent blood cancers, who have very long lifespans, can be exceedingly difficult—and the results are not always interpretable.
In this second installment of this blog series, we will focus on the OS data for PI3Kis presented by the FDA, the complexities of evaluating OS in blood cancers with long lifespans, and the broader regulatory implications of an increased focus on OS as a safety endpoint in patients with indolent diseases.
Regulatory pressure to withdraw PI3Kis continues…
The Class 1 phosphatidylinositol-3-kinases (PI3Ks) are master regulators of cell proliferation, growth, survival, motility, and immune cell function that are highly dysregulated in blood cancers. Four PI3Kis (idelalisib, duvelisib, copanlisib, and umbralisib) have been approved by the FDA for B-cell malignancies such as chronic lymphocytic leukemia (CLL), and indolent non-Hodgkin’s lymphomas (iNHL), including marginal zone lymphoma (MZL) or follicular lymphoma (FL). Please see Part 1 for additional background on PI3Kis.
As of writing this post, all accelerated approvals for PI3Kis in iNHL have been withdrawn, mostly due to a failure to complete a confirmatory trial. These withdrawals also likely reflect the ODAC decision in favor of a requirement for randomized data to support future approvals for PI3Kis (rather than single-arm trial data, which are often used to support accelerated approvals in oncology).
Currently, there are 2 PI3Kis (idelalisib and duvelisib) with full approval in later-line treatment of CLL that remain on the market.
Since the April ODAC, however, the FDA has increased pressure on sponsors to withdraw even fully approved indications for PI3Kis on the basis of a potential detriment to overall survival. The most recent development came on June 30 with a warning issued by the FDA that Secura Bio’s PI3Ki, duvelisib, may increase the risk of death when used as a third-line treatment for patients with CLL. Duvelisib received full approval for CLL in 2018 on the basis of the phase 3 DUO trial. The FDA warning stated that the agency plans to hold a future public meeting to discuss the updated overall survival data of duvelisib, and whether duvelisib should continue to stay on the market – hinting that another potential ODAC meeting may be on the horizon.
Since the April ODAC, however, the FDA has increased pressure on sponsors to withdraw even fully approved indications for PI3Kis on the basis of a potential detriment to overall survival.
“The ultimate safety endpoint”: Do PI3Kis lead to a detriment in OS?
The FDA views OS as “the ultimate safety endpoint” because it encompasses deaths directly caused by adverse events related to the drug, and deaths that might be related to long-term side effects of the drug, which can be difficult to identify. Importantly, the FDA specifies that OS “does not require [the] same statistical considerations when used as a primary safety endpoint.” The FDA’s viewpoint is straightforward: The ultimate goal with any drug therapy should be to prolong life without inflicting long-term harm. From this viewpoint, OS has a dual purpose of providing information about the effectiveness of a drug, while also informing safety.
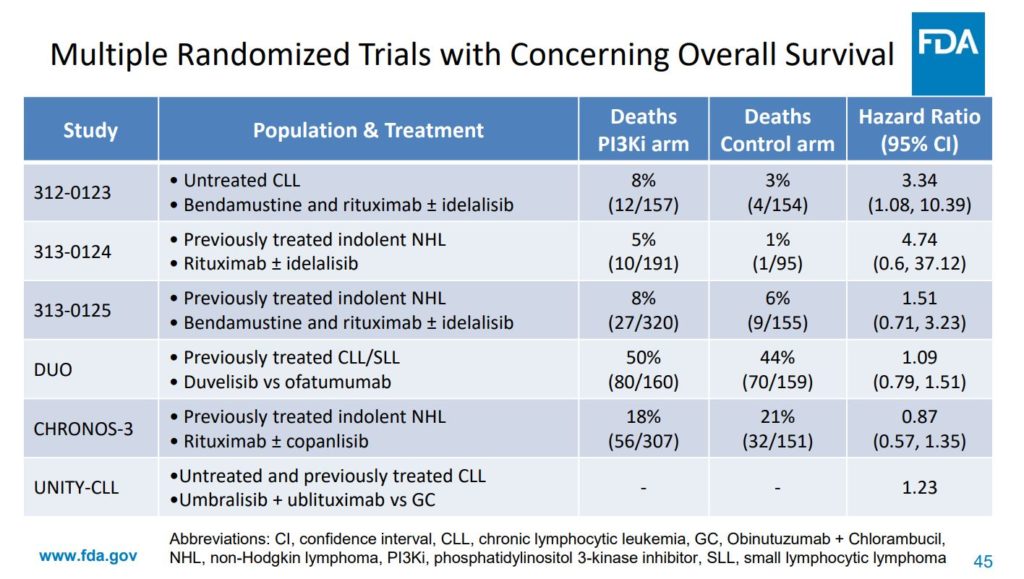
The FDA presented data at the April ODAC showing that in six phase 3 randomized trials for the approved PI3Kis, most had OS hazard ratios (HR) >1 (Figure 1) . An HR >1, based on Kaplan-Meier estimates, suggests that more patients died on the experimental arm (in this case the PI3Ki) than on the comparator arm. In 3 trials with idelalisib (the first approved PI3Ki drug), there was a much higher risk of death in the idelalisib arm, with a nearly 5× greater risk of dying in the 313-0124 trial in iNHL, and a more than 3× greater risk of dying in the 312-0123 trial in CLL.
The FDA views OS as “the ultimate safety endpoint” because it encompasses deaths directly caused by adverse events related to the drug, and deaths that might be related to long-term side effects of the drug, which can be difficult to identify.1
The OS results in trials with other PI3Kis across various patient populations and treatment regimens (DUO, CHRONOS-3, and UNITY CLL) did not show a survival imbalance as extreme as that observed in the idelalisib trials. Although most of these trials exhibited OS HRs >1, the 95% confidence interval was very wide and included 1. The CHRONOS-3 trial of copanlisib in iNHL was an exception, with an HR of 0.87 (95% CI: 0.57, 1.35) (Figure 1).
The FDA interprets these data to indicate an overall pattern of potential detriment to survival in patients treated with PI3Ki as a class, possibly linked to an increased risk of infection or immune-mediated adverse events, or unidentified long-term effects of PI3Kis that may negatively impact the efficacy of subsequent therapies.3
Imbalances in OS are not unheard of in blood cancer clinical trials…
The FDA repeatedly describes a pattern of detriment in survival with PI3Kis as “unprecedented” in oncology, but are unfavorable imbalances in OS in blood cancer trials really unprecedented? A quick review of the literature disproves this notion.
The Bruton’s tyrosine kinase inhibitor (BTKi) ibrutinib was approved for previously untreated CLL in January 2019 on the basis of the iLLUMINATE trial. At the final analysis from iLLUMINATE, there was an OS HR of 1.08 in favor of the comparator arm. Similarly, venetoclax, a B-cell lymphoma 2-targeted inhibitor (BCL2i), was approved for first-line CLL treatment in May 2019 on the basis of the CLL14 trial with an initial OS HR of 1.24 at the time of approval, although with 4 years of follow-up the OS HR improved to 0.85, albeit with results that were still not significant. Importantly, both ibrutinib and venetoclax are approved in multiple indications and are considered successful and paradigm-shifting drugs, despite never having shown a significant improvement in OS in blood cancers (nor have they definitively ruled out potential detriment).
These examples cast doubt on a narrative that PI3Kis are somehow uniquely detrimental to survival in indolent blood cancers. Rather, the problem with evaluating OS in blood cancer trials may be a reflection of the disease itself, rather than any particular class of drugs.
These examples cast doubt on a narrative that PI3Kis are somehow uniquely detrimental to survival in indolent blood cancers. Rather, the problem with evaluating OS in blood cancer trials may be a reflection of the disease itself, rather than any particular class of drugs.
The complexities of evaluating OS in blood cancers with long lifespans
There are several considerations that make OS data difficult to interpret in blood cancers with very long life expectancies. Most importantly, because there are few deaths, it is not feasible to appropriately power these trials to assess OS with statistical confidence. As a result, OS analyses tend to have wide confidence intervals that are highly unstable over time. For these reasons, OS is not used as a primary endpoint in indolent blood cancers. Instead, studies are typically powered for the primary endpoint of progression free-survival (PFS), which provides more clearly interpretable results. OS is often included as a secondary or exploratory endpoint, but is not usually considered conclusive.
The interpretation of OS is further challenged by trial design realities in indolent diseases; for example, patients may go on to receive several different lines of therapy before their death and trials often include a crossover arm (wherein patients on the control arm may choose to receive the experimental treatment after disease progression). Consequently, analyses of OS may be confounded and rendered uninterpretable. Finally, identifying the cause of death is fraught with difficulty when a large number of deaths may occur years after patients have discontinued study drug.
It is also worth mentioning that COVID-19 deaths present a unique challenge to interpreting OS in indolent blood cancers (and, to some extent, all clinical trials affected by the pandemic) not only because of the timing of COVID-19 infection waves and deaths, but also because of shifts in standard of care that can no longer be controlled for by randomization. Given these circumstances, it is possible, or even likely, that a pattern of OS detriment seen with the newer PI3Kis in recent clinical trials is a chance finding, rather than a real reflection of risk.
How should sponsors use OS to support benefit-risk assessments?
If it is not possible to adequately power a trial for OS or to interpret the results, how exactly should an “assessment” of OS be performed to support benefit-risk evaluation of PI3Kis? When asked this question directly by a panelist, the FDA fell back on its stance that the burden is on sponsors to prove that PI3Kis are not producing a detriment to survival – a difficult situation for drug developers. However, the FDA provided few clues as to what it is looking for (see slide 75 of the FDA presentation).
Sponsors developing new PI3Kis should be prepared to incorporate detailed analyses of the causes of death on each arm into study protocols, with the goal of providing assurance that the experimental arm is not causing excess deaths related to immune-mediated toxicity or an increased risk of infection due to PI3K inhibition. This type of analysis would require a much more in-depth investigation than is typically done, given the problems discussed above with tracking deaths that occur long after a patient has left the study. Sponsors should also attempt to design future studies so that the OS data are better able to withstand an increased level of scrutiny. For example, trial designs that include an option to cross over to the experimental arm after progression may not be advisable.
Ultimately, even following the FDA’s suggested changes to clinical trial design, there is no guarantee that OS can be evaluated with sufficient statistical clarity to definitively show that PI3Kis are not causing a detriment to survival.
What do the experts think?
Notably, not all physicians agreed with the FDA’s conclusion of a pattern of detriment to OS with PI3Kis. In a public docket comment in response to the April ODAC meeting, Jennifer Brown, MD, PhD, “urge[d] caution in the interpretation of trials in different clinical settings,” “as well as the interpretation of long term follow-up data which may be confounded by subsequent therapy choice and crossover study design.” Dr. Brown went on to note that PI3Kis have provided “transformative and life-saving” benefits, and “in patients who are heavily pretreated, as is the case with all the existing approvals and the drugs in development, the toxicity is readily managed.”
In the context of excellent benefits in progression-free survival with PI3Kis and high unmet need for alternative therapies in heavily pre-treated patients, many physicians still view the benefit-risk profile for PI3Kis as favorable. On July 1, the CLL Society sent a letter to the FDA that received signatures of support from 40 of the top CLL/SLL physicians in the country, which urged the FDA to maintain approved PI3Kis as an option for patients with CLL:
“Going forward and looking more widely at the CLL therapeutic landscape, safety must never be compromised. But drug innovation should continue to be encouraged. We believe the FDA can leverage the power of electronic medical records and real-world data to further assess the safety of PI3K inhibitors. Delays associated with the wait for overall survival data have already started to dampen research efforts in CLL and have slowed patient access to potentially life-saving therapies. CLL is a chronic cancer, and patients are often exposed to multiple therapies over the span of their disease. Survival data will come too slowly for many patients and will never be ‘statistically pure.’ CLL Society and many others have pushed for crossover in clinical trials to ensure equipoise, which while further confounding the survival data, saves lives. In the opinion of CLL Society, clinical trial design focused on overall survival endpoints will ultimately delay or deny the best possible care to patients with CLL.”
Coming Next: Part 3 – How should dose optimization be conducted in drug classes with known immune-mediated toxicity risks?
The FDA has raised concerns that for the approved PI3Kis, dose modifications or treatment interruptions due to AEs are too common in clinical trials, indicating that the dose may be too high. The dosing regimen for all approved PI3Ki was selected based on standard, phase 1, single-arm dose escalation studies in small cohorts of patients. However, in the FDA’s view, this standard approach may lead sponsors to default to selecting the maximum tolerated dose, rather than the optimal (likely lower) dose that might achieve similar efficacy with less toxicity.
InIn Part 3 of this series, ProEd will review the panel discussion of how best to optimize drug dosing for PI3Kis, the broader FDA regulatory initiatives (ie, “Project Optimus”) surrounding dose optimization, and how these considerations may impact clinical trial design and dose-finding studies for targeted oncology drugs that modulate the immune system.
 Angela W. Corona, PhD
Angela W. Corona, PhD
Scientific Director, ProEd RegulatoryAngela is a Scientific Director for ProEd Regulatory. She is responsible for helping sponsors navigate complex regulatory communications such as FDA advisory committee meetings. She develops clinical and regulatory strategy along with high-quality scientific and medical content across a wide range of therapeutic and drug development areas. Angela received her PhD in Neuroscience from The Ohio State University and completed her postdoctoral training at Case Western Reserve University in Cleveland, Ohio.
References
- Pazdur R. The saga of PI3K inhibitors in haematological malignancies: survival is the ultimate safety endpoint. Lancet. 2022 April 14 [Online ahead of print]. https://doi.org/10.1016/S1470-2045(22)00200-5
- FDA Presentation, Introductory Comments; Presented by Nicole Gormley. Oncologic Drugs Advisory Committee Meeting. Phosphatidylinositol 3-Kinase (PI3K) Inhibitors in Hematologic Malignancies. April 21, 2022. https://www.fda.gov/media/157837/download
- FDA Briefing Document. Oncologic Drugs Advisory Committee Meeting. Phosphatidylinositol 3-Kinase (PI3K) Inhibitors in Hematologic Malignancies. April 21, 2022. https://www.fda.gov/media/157762/download
- Moreno C, et al. First-line treatment of chronic lymphocytic leukemia with ibrutinib plus obinutuzumab versus chlorambucil plus obinutuzumab: final analysis of the randomized, phase 3 iLLUMINATE trial. Haematologica. 2022 Jan 13 [Online ahead of print]. https://doi.org/10.3324/haematol.2021.279012.
- Fischer K, et al. Venetoclax and obinutuzumab in patients with CLL and coexisting conditions. N Engl J Med. 2019;380(23):2225-2236. https://pubmed.ncbi.nlm.nih.gov/31166681/
- Al-Sawaf O, et al. Minimal residual disease dynamics after venetoclax-obinutuzumab treatment: extended off-treatment follow-up from the randomized CLL14 study. J Clin Oncol. 2021;39(26):4049-4060. https://pubmed.ncbi.nlm.nih.gov/34709929/
