Communicating the Complexities of Subgroup Analyses at an AdCom
Within clinical trials, exploratory or post-hoc subgroup analyses are widely recognized as only “hypothesis generating” due to their high potential for bias and/or misleading interpretation. This is the main reason why Sponsors cannot make efficacy claims or seek regulatory approval based on evidence of efficacy in a certain subgroup unless that benefit is consistent with the broader trial population and unless the trial is positive overall for the intention-to-treat (ITT) population. This begs the question, “Is it acceptable to use an exploratory subgroup analysis to restrict an indicated population when the data suggest less benefit in a particular subgroup?”
That is exactly what FDA asked the Oncologic Drugs Advisory Committee (ODAC) to consider in the case of the PROpel data, based on their conclusion that the combination of olaparib plus abiraterone has a favorable benefit/risk only in the subgroup of patients with advanced prostate cancer who test positive for a mutation in the BReast CAncer (BRCA) gene, which regulates homologous recombination repair of DNA. However, one might argue that the exploratory/post-hoc analysis on which FDA based their conclusion remains, by its very nature, fraught with potential for bias and/or misleading interpretation and is thus only hypothesis generating.
“Is it acceptable to use an exploratory subgroup analysis to restrict an indicated population when the data suggest less benefit in a particular subgroup?”
In the era of precision medicine, we expect that treatment choices are driven by biomarkers that can predict clinical benefit. In the case of poly ADP-ribose polymerase (PARP) inhibitors, like olaparib, BRCA mutations or deficiencies in homologous recombination repair (HRR) can predict clinical benefit. But there may be clinical situations where biomarker testing is limited or where patients without BRCA mutations might benefit from treatment with a PARP inhibitor. Indeed, the science suggests that patients with metastatic castration-resistant prostate cancer (mCRPC) may benefit from the combination of a PARP inhibitor with an antiandrogen, like abiraterone, regardless of BRCA mutation status, based on the synergistic activity of these 2 drug classes. In addition, the majority of patients with mCRPC (especially in disadvantaged communities) do not have definitive biomarker testing for BRCA mutations, usually due to cost and/or lack of available tumor tissue. That is the context for the PROpel study investigating the combination of the PARP inhibitor olaparib (Lynparza) plus abiraterone (Zytiga) as first-line treatment of mCRPC.
The PROpel trial was designed to assess the activity of this combination in the broad, unselected, ITT population, and data on BRCA mutation status by ctDNA and tissue tests were collected for the purpose of exploratory subgroup analysis. The trial met its primary endpoint in the ITT population, demonstrating a statistically significant 40% improvement in radiologic progression-free survival (rPFS). Therefore, AstraZeneca was seeking a broad indication that includes BRCA mutant, BRCA wild-type, and BRCA unknown patients. The Sponsor also presented evidence that patients without BRCA mutations or with unknown BRCA status benefited from the combination of olaparib plus abiraterone. However, on April 28, 2023, the ODAC voted 11 to 1 (with 1 abstention) to limit use of the combination to men whose tumors tested positive for a BRCA mutation, which represents only about 10% of patients with mCRPC. This was based on post-hoc subgroup analyses that created the perception of a less favorable benefit/risk in the BRCA wildtype or unknown patients.
On April 28, 2023, the ODAC voted 11 to 1 (with 1 abstention) to limit use of the combination to men whose tumors tested positive for a BRCA mutation
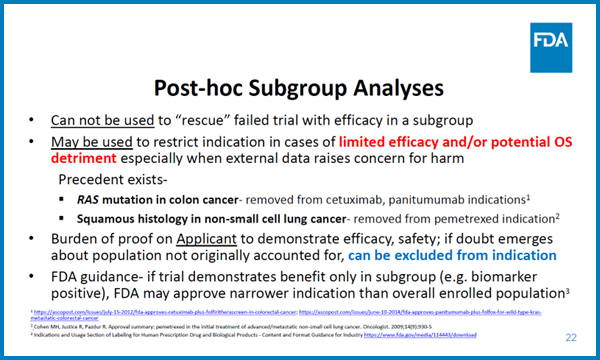
Dr. Chana Weinstock articulated the FDA’s position on this issue at the April 28 ODAC meeting. She said that the Agency discourages using subgroup analysis to try to argue for efficacy in a specific group, particularly in a failed trial (although PROpel was a positive study). However, she highlighted historical precedent for limiting indications based on post-hoc subgroup analysis suggesting that certain subgroups might have compromised safety or a potential overall survival detriment. Finally, she cited the FDA guidance that states that if a trial only shows benefit in a selected subgroup, the indication may be limited to a narrower population, especially if that same signal is observed in other comparable trials. (Figure 1)
Figure 1
Jorge Nieva, section head of solid tumors at the University of Southern California, objected to restricting the indication to only those patients with known BRCA mutations, saying “I worry that the approach used in this application can justify removing any subgroup from any application where that subgroup has an OS curve that crosses one. FDA seems to be looking at these OS curves in a vacuum and is ignoring the corroborating evidence that some non-BRCA patients could benefit significantly.”
“I worry that the approach used in this application can justify removing any subgroup from any application where that subgroup has an OS curve that crosses one.”
It is common for Sponsors to find themselves in this situation at ODAC where the data are somewhat ambiguous and the arguments/counter arguments are highly statistical in nature. This is especially true for subgroup analyses. The key communication goal when addressing an advisory committee is to make your position as easy to understand as possible by breaking down your argument into digestible bites. If your messages are too complex, statistical or philosophical, the committee may not fully appreciate your position. When this occurs at ODAC, the committee typically defers to the FDA’s position.

Aaron Csicseri, PharmD
Senior Scientific Director
Dr. Csicseri joined the ProEd team in November 2017 as a scientific director, responsible for scientific leadership, content development, strategic input, and effective moderation of team meetings. Aaron received his PharmD at the University of Buffalo, where he studied the clinical curriculum. He has 10+ years of experience as a medical director/clinical strategist in the accredited medical education field (CME), as well as in the non-accredited PromoEd sphere. Over the past 5 years, he has been guiding Sponsor teams in their preparations for FDA and EMA regulatory meetings in a wide variety of therapeutic areas. Aaron is based in Grand Island, NY, just outside of Buffalo, New York.
Connect with Aaron on LinkedIn.